Root Canal Treatment in Turkey: Expert Care in Antalya
For a better understanding of root canal treatment, it is useful to have some information about the general structure of the tooth.
Sections and structural layers of a tooth:
External parts of the tooth:
Crown:
It is the upper part of the tooth visible in the oral cavity. It is covered with enamel and is the hardest tissue of the body
Cervix:
It is the transition area between the crown and the root at the gum line. The enamel-cement junction line is located here. In case of gum recession, it is exposed, and sensitivity may occur.
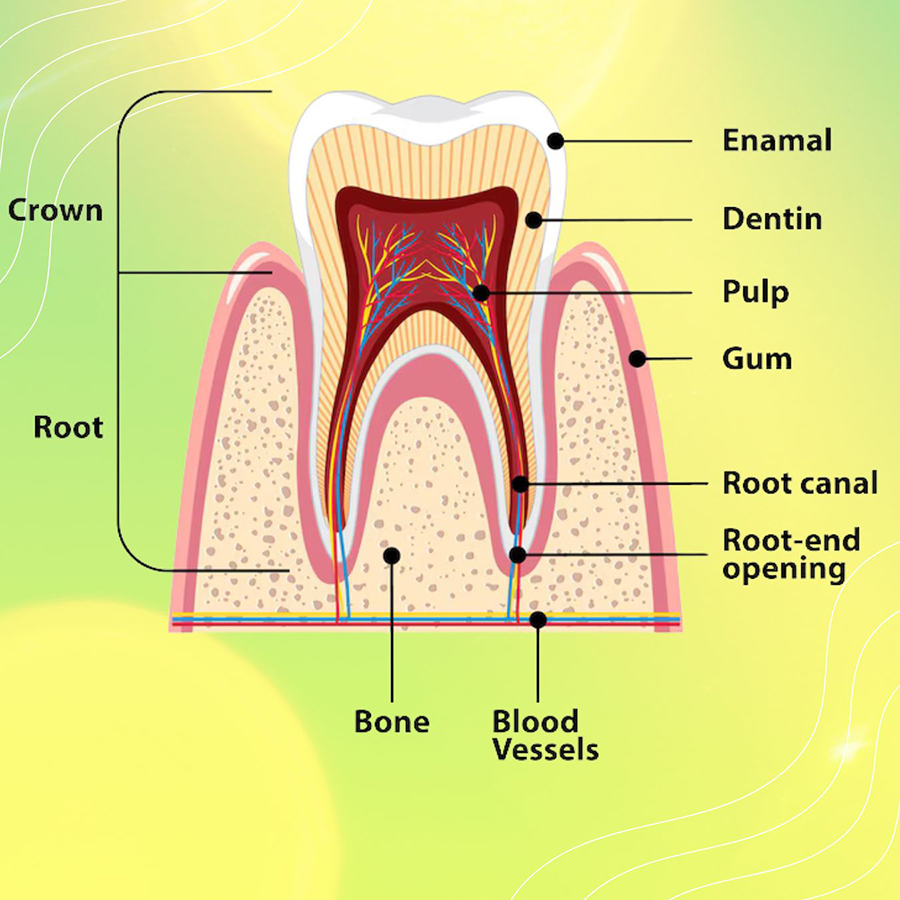
Radix - Root
It is the part embedded in the jawbone (alveolar bone), covered with cementum, and connected to the bone with periodontal ligament.
- Single root: incisors, canines, premolars (some).
- Double root: Lower molars (with two roots).
- Triple root: Upper molars (two cheek roots, one palatal root)
Internal layers of the tooth
Enamel:
Enamel contains calcium phosphate and is the most mineralized tissue of the body. It is colored and translucent, reflecting the color of the underlying dentin. It is resistant to acid erosion and caries but does not regenerate.
Dentin:
It is found under the enamel and under the cementum on the root surface. It contains 70% minerals, 30% organic matter, and water (softer than enamel). It contains microscopic canaliculi, and these canaliculi extend to the pulp and cause hot/cold sensitivity.
Pulp:
It is the living centre of the tooth and contains
- Blood vessels (provide nutrition),
- Nerves (gives pain sensations),
- Lymphatic vessels (immunity),
- Odontoblasts (dentin-producing cells).
- The pulp chamber (in the crown) and root canals (along the root).
If infected with caries, root canal treatment is required.
Cementum:
It is a bony layer covering the root surface. It contains 65% minerals (softer than enamel and dentin). Periodontal ligament fibers are attached here. If it is exposed in gingival recession, the root surface becomes sensitive.
Periodontal Ligament (PDL):
Elastic fibers connecting the tooth root to the alveolar bone. It absorbs shock by absorbing chewing pressure and provides proprioception (adjusts the bite force).
Support tissues surrounding the tooth:
Gingiva:
It is covered with pink, keratinized mucosa. Healthy gums are firm and do not bleed. In case of periodontitis (gum disease), gum recession occurs.
Alveolar bone:
It is the jawbone that surrounds the roots of the teeth. When the tooth is extracted, it begins to dissolve (a bone graft may be required for an implant).
Nerve and vascular network:
Vessels/nerves entering and leaving the pulp pass through the jawbone. Branches of the trigeminal nerve provide sensory transmission to the teeth.
Root canal treatment is a dental procedure in which the infected or inflamed pulp inside the tooth is removed. This is usually done to prevent tooth extraction when the pulp (the tooth's nerve) is irreversibly damaged (inflamed or dead) for various reasons. The main goal of the treatment is to completely remove the damaged pulp, clean and shape the root canal system thoroughly, and then fill it.
Reasons for the need for root canal treatment:
Cavities:
Tooth decay is one of the main sources of threat to the pulp. The most common cause of infection in the canals is the bacterial effect of caries. Deep caries or large cavities can lead to infection of the pulp.
- Initially, caries affects only the enamel, but as it progresses, it reaches the dentin layer and eventually the pulp.
- Bacteria that reach the pulp due to caries lead to inflammation (pulpitis) and abscess formation.
- Caries that can be solved with a small filling may require root canal treatment if neglected.
Gum Diseases (Periodontitis)/Infections:
In advanced gum disease, bacteria can spread from the gum pockets to the root surface and root canals. In rare cases, gum infection can enter the tooth through the root tip.
Trauma:
In cases such as sports accidents, falls, or fights, the tooth may lose its vitality. Chronic Trauma (Teeth Grinding - Bruxism): Constant pressure can lead to wear of the pulp.
Tooth fractures or cracks:
- A tooth can be broken as a result of a fall, a blow, or biting down on something hard. If the fracture line reaches the pulp, there is a risk of infection.
- Even invisible cracks allow bacteria to seep in over the long term.
- In severe trauma, the blood supply to the pulp is interrupted, the tooth dies, and infection may develop.
Abrasion or erosion:
- Acidic foods/drinks or stomach acid (reflux) erode the tooth enamel, exposing the dentin.
- Hard tooth brushing or clenching can damage the dentin layer.
Recurrent dental treatments:
- Filling the same tooth repeatedly, interventions close to the pulp may cause irritation of the nerve.
- An incorrect filling can damage the pulp by pressing on the tooth.
- If decay occurs under fillings or crowns, infection can spread.
Signs of the need for root canal treatment:
- Severe toothache that wakes you up at night
- Hot/cold sensitivity and persistence of pain for a long time
- Pain when chewing or pressing
- Gingival swelling, abscess or fistula (purulent wound)
- Tooth discolouration (grey or dark yellow)
- Throbbing sensation for no reason
Clinical examination:
- Facial swelling, asymmetry, lymph nodes, and jaw joint examinations are performed.
- General oral hygiene, appearance of the mucosa, contour, texture (hardness, fluctuation), color, presence of fistula, crown structure of the tooth, and tissue loss due to caries or trauma are examined.
- The restorability of the tooth after treatment (restorability) is evaluated before the treatment decision is made.
Special tests:
- Pulp Tests: It is performed to evaluate the vitality of the pulp. The most commonly used are thermal tests (cold/hot).
- Percussion Test: Usually performed with the handle of a mouth mirror. This test shows whether the periodontal supporting tissue is healthy.
- Transillumination and biting devices can be used for crack detection.
Radiographic imaging:
- Periapical X-ray (PA): It is the most commonly used method. A single tooth and root tip (periapical region) are visualized in detail.
- Panoramic X-ray (OPG): The whole jaw and teeth are examined in a single image.
- Computerized tomography (CT-CBCT): Provides 3-dimensional (3D) imaging.
- Bite-wing x-ray: It allows the back teeth to be visualized without overlapping.
- Digital radiography: Digital sensors are used instead of conventional film.
Anesthesia for root canal treatment:
- Firstly, local anaesthesia is performed to completely numb the tooth and surrounding tissues
- Thanks to modern anaesthetic agents, no pain is felt during the procedure
- Different injection techniques can be used to increase the anaesthetic effect, especially in infected teeth
- After checking that the anaesthesia effect has fully started, the procedure is started
Isolation of the tooth to be treated:
To ensure a sterile working environment, the tooth to be treated is isolated with a special latex or latex-free cover (rubber dam). This application prevents saliva and bacteria from reaching the treatment area while providing the physician with a drier and cleaner working area. It also increases the safety of treatment by eliminating the risk of swallowing small instruments. It is fixed to the tooth with special clamps, ensuring that it remains in place throughout the procedure.
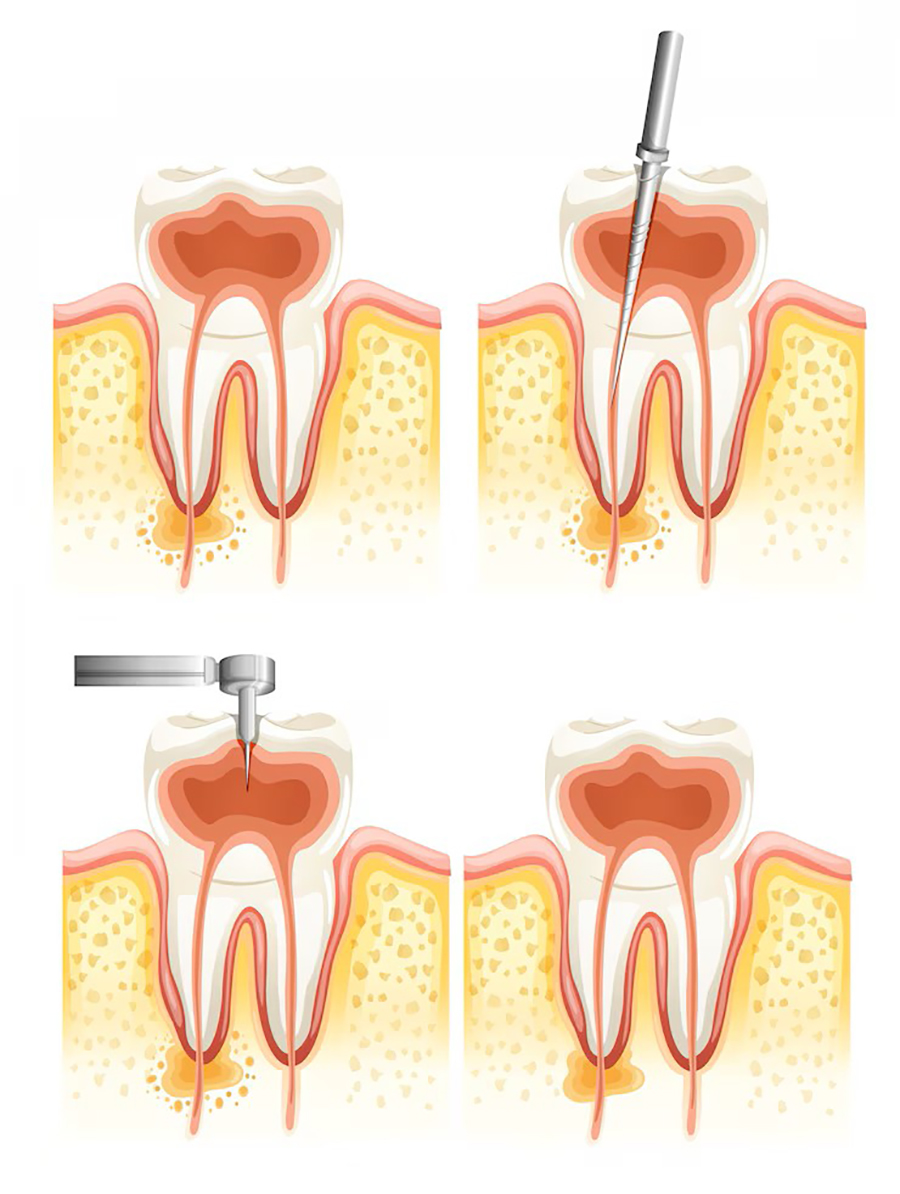
Accessing the pulp chamber of the tooth (opening an accessory cavity):
- A hole is drilled in the tooth to gain access to the root canal system. Access is determined by ‘the size and shape of the pulp chamber and the position of the canal orifices.
- Using high-speed hand tools and specialized burs, the pulp chamber is accessed through the chewing surface of the tooth. At this stage, special accessory burs designed in accordance with the anatomy of the tooth are used.
- Through the opened cavity, the infected pulp tissue is reached, and the entrances of the root canals are determined. In clinics where a microscope is used, this process is performed much more precisely.
Canal cleaning and widening:
Using hand files of various sizes and nickel-titanium rotary instruments, the infected dentin layer is removed from the canal walls. At this stage, the canal shape is optimized and widened. During the procedure, the canal length is continuously checked with an electronic apex locator. X-rays are taken periodically when necessary to confirm the accuracy of the procedure.
Canal disinfection:
Bacteria are inactivated by washing with sodium hypochlorite solution. Saline or distilled water can be used for the final washing. In advanced technology clinics, more effective sterilization can be achieved by applying ultrasonic activation or laser-assisted disinfection methods.
Canal filling (canal obturation):
After the canal is completely dried, it is filled with a rubber-like material called gutta-percha. In addition, a special canal paste (usually a zinc oxide core) is used to ensure that every point of the canal is tightly closed. Filling can be done in various ways, such as lateral condensation, thermoplastic techniques, or the single-cone method. The success of this stage directly affects the long-term success of the treatment.
Restoration of the tooth superstructure:
After root canal treatment, the superstructure of the tooth is restored with appropriate materials. While composite filling may be sufficient in small material losses, post-core application may be applied, or a porcelain crown may be required in large material losses. Direct composite restorations may be preferred in aesthetic area teeth. The quality of the restoration significantly affects the functional life of the tooth.
The duration of root canal treatment depends on the condition of the tooth and the technology used:
Single-session treatment:
It is applied in cases of live pulp (as a result of trauma), small infected teeth, and anterior teeth (single-rooted). It requires fewer clinic visits, patient comfort is high, and the risk of infection is low.
Two-session treatment (most common practice):
It is applied in large infected teeth, multi-rooted molars, and in the presence of apical lesions.
Session 1:
- Cleaning and disinfection
- Temporary filling application
- 5-7 days waiting time
Session 2:
- Channel filling
- Permanent restoration
Cases requiring three or more sessions:
If there is a very large area of infection, if the canal anatomy is complex, if there is a suspicion of fracture in the tooth, or if antibiotic treatment is required. Session intervals are usually 1-2 weeks.
Which tooth takes how many sessions in root canal treatment?
| Tooth Type | Average Number of Sessions | Treatment Duration |
|---|---|---|
| Front Teeth | 1-2 | 30-50 minutes |
| Premolars | 1-2 | 45-60 minutes |
| Premolars | 2-3 | 60-90 minutes |
| Retreatment | 2-4 | Longer |
Possible complications:
- If your tooth has an unusual shape, root canal treatment may cause holes in the side of the tooth root that will require further treatment.
- Root treatment may not be very successful if there is a prolonged or severe infection (e.g., a tooth abscess).
- There is a risk of forced expulsion of debris, dentin chips, irrigation solution, and microorganisms through the apical foramen, especially when the instrument size is approximately the same as the apical portion of the root canal.
- Procedural errors such as instrument separation, ledging, zipping, elbow formation, perforation, and loss of working length may occur.
- Loss or deterioration of the temporary filling.
- Pain or discomfort may persist or occur after treatment.
- Failure to completely eradicate the infection.
- The treated tooth may lose its original whiteness and become darker.
Things to consider after root canal treatment:
Points you should pay attention to for the longevity of your treatment and a comfortable healing process:
First 24-48 hours :
- Do not eat until the anaesthetic effect wears off (2-4 hours)
- Do not chew on the treated tooth for the first 24 hours
- Avoid hot food/drinks (may cause bleeding)
Pain management:
- Painkillers containing paracetamol can be used for mild pain
- In case of severe pain, contact your dentist
- Pain lasting longer than 3 days requires control
Nutrition:
- Prefer soft foods on the first day (puree, yoghurt, soup)
- Avoid hard and sticky foods (chewing gum, nuts)
- Do not consume acidic drinks
Oral care
- Do not brush for 12 hours after treatment
- Then use a soft bristle brush
- Be careful when flossing (do not overdo it)
Smoking and alcohol use:
- Do not smoke for the first 48 hours (delays recovery)
- Alcohol consumption can interact with anaesthetics
Paying attention to the temporary filling:
- If the temporary filling falls out, contact your doctor as soon as possible
- Prevent the filling from breaking by avoiding hard foods
Control appointments:
- After 1 week, go for a follow-up appointment
- After 6 months, have a follow-up X-ray
- The condition of the tooth should be monitored with annual checks
Unusual circumstances
If you experience the following conditions, contact your dentist immediately:
- Severe swelling
- Fever and malaise
- Throbbing that does not pass
- Tooth mobility (swaying)
Root canal treatment is generally a safe procedure, but in some cases it may not be possible or may require special precautions. People and situations that may not be able to have root canal treatment:
The tooth is damaged beyond salvage:
Treatment may fail if the roots are severely fractured, there is extensive decay, or the tooth has lost its supporting tissues. Alternatives such as tooth extraction and implants should be considered.
Bone loss and advanced periodontal disease:
Severe loss of the bone tissue surrounding the tooth prevents the tooth from holding in the long term. Periodontal treatment may be required first; if the condition worsens, the tooth may be extracted.
Excessive complexity of canal anatomy:
In some teeth, root canals may be extremely narrow, curved, or inaccessible. Surgical intervention (apicoectomy) or extraction may be recommended.
Those with serious systemic diseases:
- Uncontrolled diabetes (impairs the healing process)
- Diseases that weaken the immune system (HIV, chemotherapy)
- Risk of infection in patients with heart valve prosthesis
- Physician consultation is essential; antibiotic prophylaxis may be required.
First and last trimester of pregnancy
If it is not urgent, elective procedures are postponed to protect the fetus. It can be safely performed in the second trimester (4-6 months).
Those at risk of allergic reactions:
- History of allergy to latex, anesthetic agents, or canal filling materials.
- Alternative materials can be used.
Psychologically unprepared patients:
Patients with extreme dental anxiety or phobia may be treated under sedation or general anesthesia.
Excessive calcification of roots in elderly patients:
Blockage of the root canals by calcification may make treatment technically impossible. There may be a surgical approach or extraction.
Those who postpone treatment for economic reasons:
In case of emergency infection, the tooth can be extracted after the infection is treated, and then an implant can be planned.
Patients who cannot adapt to the treatment:
Short-term interventions can be performed under general anesthesia in cases that prevent movement control, such as severe dementia and Parkinson's disease.
Root canal treatment prices vary from country to country and from clinic to clinic. However, according to general market averages, approximate prices are as follows in euros:
| Country | Root Canal Treatment Prices (Euro) |
|---|---|
| Turkey | 150 € – 350 € |
| UK | 400 € – 800 € |
| USA | 700 € – 1,200 € |
What happens if root canal treatment is not performed?
When a tooth requiring root canal treatment is left untreated, symptoms and/or infection may persist, and the end result is usually extraction. The goal of treatment is to save the tooth and allow it to continue to function.
Is there pain during root canal treatment?
- Thanks to strong local anaesthetics, you will not feel any pain during the procedure
- Special anaesthesia techniques (such as intraligamentary injection) are applied, especially in infected teeth
- Sedation options available for sensitive patients
Is there pain after root canal treatment?
- Mild tenderness is normal (may last 1-3 days)
- The majority of patients do not experience severe pain
- Can be easily controlled with prescribed painkillers
Is there swelling after root canal treatment?
Mild swelling is normal. However, if there is severe swelling, fever, or throbbing pain, the dentist should be consulted immediately. This may be a sign of infection.
Are root canal-treated teeth durable?
Root canal-treated teeth are not as durable as normal teeth. It is recommended to apply protective crowns, especially on the back teeth.
What is the lifespan of root canal-treated teeth?
With proper care and protection, these teeth can remain in the mouth for a lifetime.
What is the difference between root canal treatment and filling?
- Filling: In superficial caries, only the damaged part of the tooth is cleaned and filled.
- Root Canal: In deep caries reaching the nerve, the inside of the tooth is completely cleaned and the root canal is filled.
Is there an age restriction for root canal treatment?
There is no definite age restriction for root canal treatment, but special cases are taken into consideration. The condition of the tooth, the general health status of the patient, and oral hygiene play a more decisive role than the age factor.
Is root canal treatment performed in children?
Yes, a partial root canal treatment called ‘pulpotomy’ can be applied to deciduous teeth. This is important for the health of permanent teeth.
In deciduous teeth:
- Applicable if root resorption has not started
- Particularly favoured in cases where early loss would be detrimental
- Can be performed in suitable cases from 3-4 years of age
Is it necessary to use antibiotics before root canal treatment?
If there is only active infection (abscess, swelling), your physician may prescribe antibiotics for 3-5 days.
Is laser used in root canal treatment?
Yes, in some clinics, laser-assisted root canal treatment can be performed for disinfection. This method provides more effective cleaning and accelerates healing.

